If You've Ever Taken Antibiotics You Need To Read This
Why you can trust Nutri Advanced Every article on our site is researched thoroughly by our team of highly qualified nutritionists. Find out more about our editorial process.
Whilst antibiotics can be a real lifesaver, they can also bring with them unwanted side effects. Antibiotics cannot distinguish between good and bad bacteria so indiscriminately wipe out both. Once both good and bad have been wiped out, harmful bacteria quickly proliferate and problems can soon start to arise. This disruption to the microbiome is known as dysbiosis. A dysbiotic microbiome may not perform vital functions such as nutrient supply, vitamin production and protection from pathogens. It has also been associated with a large number of health problems and chronic conditions.1
Antibiotic use is the most common and significant cause of major decreases in healthy gut bacteria and the overgrowth of harmful bacteria.
Antibiotics have also been associated with the development of unwanted gastrointestinal symptoms and even IBS. Antibiotic-associated diarrhoea is a common side effect of antibiotic use affecting up to 30% of adults and 40% of children and may occur between the initiation of therapy and up to 2 months after treatment stops.
Antibiotic-associated diarrhoea is thought to be the direct result of disturbance in the normal intestinal microflora, in particular infection with the harmful bacteria Clostridium difficile. Antibiotic eradication of beneficial bacteria in the gut enables Clostridium difficile to flourish.
However, there are a few things you can do to help minimise disturbances to the gut microbiome should you need to take an antibiotic.
If you need to take antibiotics and do experience unwanted side effects, supplementation with Saccharamoyces boulardii can be an effective way to relieve symptoms. Saccharomyces boulardii is a non-pathogenic yeast which has been shown to help support a healthy balance of flora. It is also resistant to antibiotics and can be recommended to patients whilst they are receiving antibiotics. Saccharomyces boulardii has been shown to be effective against harmful bacteria associated with antibiotic side effects such as Clostridium difficile. The effectiveness of Saccharomyces boulardii for the prevention of antibiotic side effects has been demonstrated in a number of clinical trials and meta-analyses2,3.
Even if you don’t experience any obvious side effects during antibiotic therapy, it is still important to supplement with a high quality probiotic supplement once you have finished your course. This is to help replenish a healthy balance of microflora to reduce the risks of longer term effects.
✓ Choose Specific Probiotic Strains
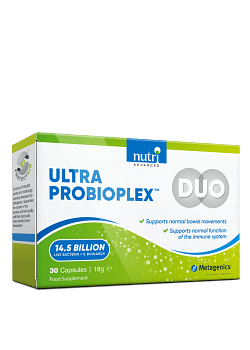
Choose a probiotic supplement that contain a high level of specific strains that are comprehensively studied and have been shown to be effective. Some of the most comprehensively studied strains include Lactobacillus acidophilus NCFM®, Lactobacillus paracasei lpc-37, Bifidobacterium lactis Bi-07, and Bifidobacterium lactis Bi-04. This specific combination of strains, when taken at the same time as antibiotics, has been shown to minimise disturbances to the gut microbiota and reduce those all-to-frequent side effects. To find out more read our summary of the study here.
✓ Diet
It is also important to be particularly careful with your diet whilst using antibiotics and afterwards too. Consume plenty of prebiotic foods, including asparagus, artichokes, bananas, onions, garlic, apples, beans & lentils, that will help the good bacteria to repopulate and avoid refined, sugary foods to limit the growth of unhealthy microorganisms. Probiotic-rich foods should also be consumed, especially after a course of antibiotics, to up your intake of good bacteria. Fermented foods such as kefir, kimchi, tempeh, lassi, sauerkraut and kombucha naturally contain high levels of a variety of beneficial bacteria and are a great addition to your daily diet.
References:
1. Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. BioMed Central. 2016 April; 8:39
2. Czerucka D, Piche T, Rampal P. Review article: yeast as probiotics – saccharomyces boulardii. Aliment Pharmacol Ther. 2007 Sep 15;26(6):767-78
3. Tung JM, Dolovich LR, Lee CH. Prevention of Clostridium difficile infection with saccharomyces boulardii - a systematic review. Can J Gastroenterol. 2009 Dec;23(12)817-21
This website and its content is copyright of Nutri Advanced ©. All rights reserved. See our terms & conditions for more detail.
Nutri Advanced has a thorough research process and for any references included, each source is scrutinised beforehand. We aim to use the highest value source where possible, referencing peer-reviewed journals and official guidelines in the first instance before alternatives. You can learn more about how we ensure our content is accurate at time of publication on our editorial policy.
Most Popular Articles
-
7 Surprising Ways To Support Your Magnesium
If you are displaying signs of a magnesium deficiency, here are 7 ways to boost your magnesium levels that are easy to incorporate into your daily life. -
5 Best Vitamin C Supplements Picked By Our Experts
Learn more about the different types of vitamin C, the different benefits you get from different types, and what you get for spending more on a good supplement. -
Top 5 Vitamins For Energy And Tiredness Picked By Our Experts
The 5 best and most important vitamins for energy & tiredness including B vitamin food sources & best supplement forms for energy. -
Benefits of Myo-Inositol for Polycystic Ovary Syndrome (PCOS)
In this research review article, we take a closer look at a lesser-known natural compound called myo-inositol that has been found to have significant potential to improve many of the prevalent features of PCOS. -
Top 10 Reasons to Give Your Kids Omega-3
Read the top 10 reasons that kids should have plenty of Omega-3- an essential fatty acid- including for depression, brain function, sleep & reading/maths skills.